(from Eric)
One of the obvious differences in practicing medicine in Africa versus the USA is that there are diseases that you have to master here that you wouldn't know how to treat had you not come. Foremost among these is malaria. Despite a few locally acquired cases in Florida and Texas this past summer, malaria is basically unheard of in the United States. At the end of medical school in the US, I had learned some about the disease, but only really on a theoretical level. I had forgotten most of what I learned, and certainly had no practical experience.
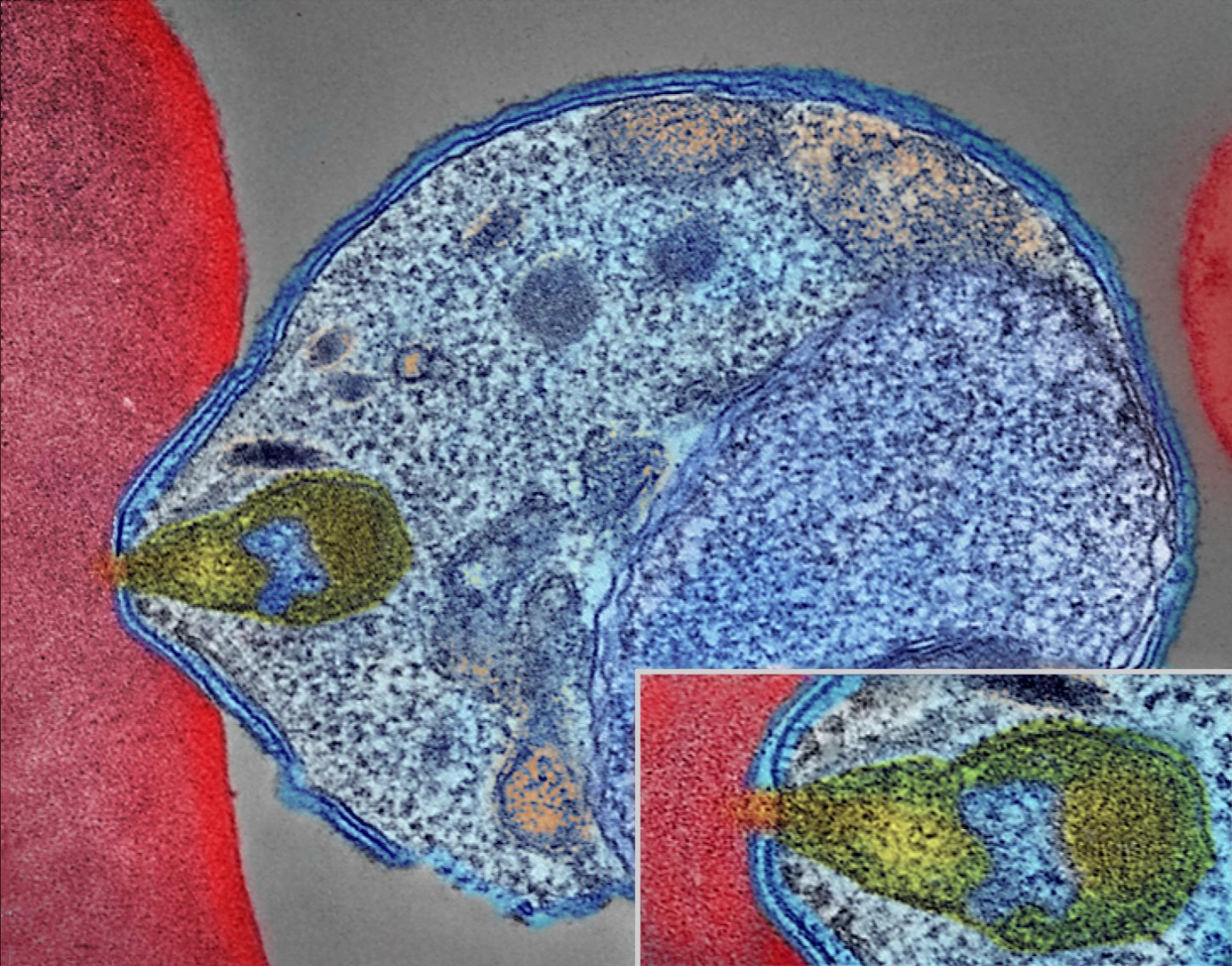 |
| Malaria parasite infecting a red blood cell |
Here in Burundi, for many years, malaria was my number one diagnosis. As in, more than 50% of my patients were admitted with some severe complication of malaria such as kidney failure, severe anemia, or a deep coma. Many of them died, but because of good treatments that are available, most of them could live and their recoveries were sometimes quite dramatic (and very gratifying!). It's a complicated disease, and so it was probably the disease that I spent the most time teaching my medical students about.
Malaria is around all year, but it is also highly seasonal. I think it was 2017 and 2018 that Burundi declared back-to-back epidemics (with 2019 numbers being quite high but no epidemic officially announced). The number of cases was more than 80% of the total population. Most everyone was getting malaria. Many people got it multiple times in the same season. Then, starting in 2020, the epidemic rates seemed to be decreasing.
Enter 2023: This year, we have had virtually no malaria.
We are now at the end of the would-be "malaria season" and yet the numbers never rose. Less than 1% of our tests are positive. I have no malaria patients on my service, and because of the significant contribution this disease makes to hospital census, for the first time since our team arrived, instead of a steady rise in patients numbers, hospitalizations are actually down.
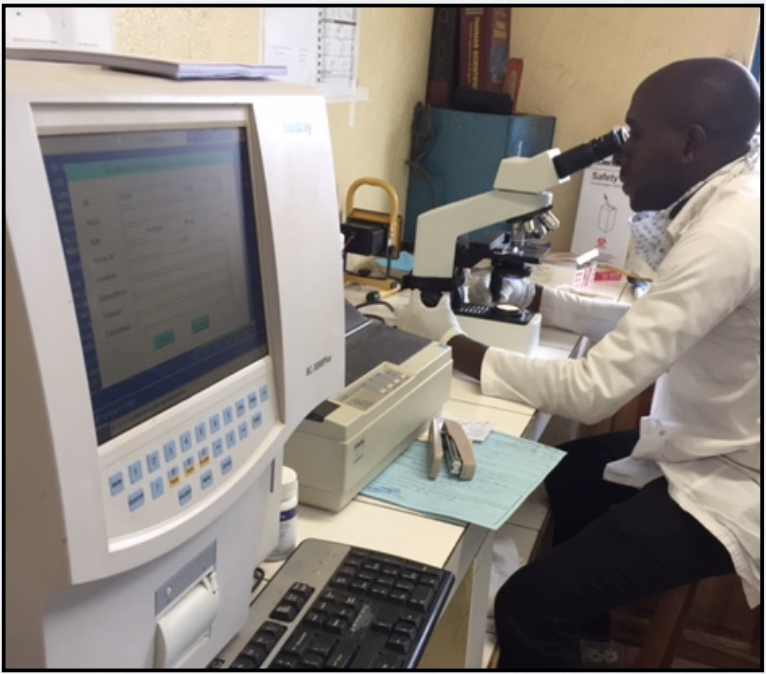 |
| Kibuye's head lab tech performing malaria microscopy |
What happened? Good question. There are very effective malaria prevention strategies, including indoor residual spraying and distribution of insecticide treated bed nets. There is a national malaria program that is hard at work, but as far as I know, they were hard at work even when Burundi was suffering repetitive epidemics. Médecins Sans Frontières (i.e. "Doctors without Borders") provided a great service to our hospital for a couple years, paying for treatment of all patients hospitalized for severe forms of the disease. But it seems hard to understand how that effort would result in so much prevention.
Christianity refers to an idea called "common grace". This is a characteristic action of God, who sends rain and sun on everyone, the evil and the good, the just and the unjust (Matthew 5:45). Across the country, Burundi has experienced common grace in the reduction of malaria this year. Long may it last.
It strikes me that this situation demonstrates two characteristics of common grace. First, it is mysterious. Why did this happen? Is there a direct cause? Nothing leaps to the eye. But understanding something is not a prerequisite for being thankful for it. Second, it is easy to overlook. Being thankful for the absence of something is not what any of us are good for. Something amazing has happened to Burundian health this year, yet we are all prone to overlook it because it is something amazing that did not happen. It gives me pause to think what other grace in my life might be mysterious or invisible enough for me to overlook it.

What a blessing!!
ReplyDelete