29.4.22
A Reflection on Psalm 46
22.4.22
Resurrection Hope
by Rachel
Happy Easter from the Serge Kibuye team! We spent the day together as a team, as we always do, feasting at a brunch potluck with our Burundian neighbors, worshipping together, and finally hunting for Easter eggs. I love these small and large team traditions, and the passing of Good Friday death into Easter Sunday resurrection in community.
The events of the weekend gave me a chance to think about resurrection…about Jesus’ resurrection and our hope, as Christians, of eternal life. But also about all the small moments of resurrection and redemption that we see around us all the time, if we have eyes to see. I was reflecting mainly on a special story that I got the privilege to be a part of last month. Eric and I shared part of this story doing our time in the US in 2018, so if you got the chance to be at one of our presentations, the story might sound familiar to you, too.
Triphonie first came to see me at the end of her fourth pregnancy, about seven years ago now. Her baby had died before being born, and upon investigating a bit more, I found out that she had no living children. All of her first four pregnancies had resulted either in the baby dying before labor (in the last 1-2 months of pregnancy), or stillbirth, where the baby died during or shortly after labor. It was devastating for her, and difficult for us as the medical team to be a part of as well. I asked her to come and see me during her fifth pregnancy in hopes that it would end differently. Many times in Burundian medicine, we are shooting in the dark, without tests and labs to guide us, unsure of a diagnosis, trying treatments that aren’t necessarily proven to be of strong benefit. This was the case with Triphonie. But we did simple interventions: a monthly ultrasound, aspirin and vitamin tablets, steroids to help the baby’s lungs mature, and ultimately a Cesarean delivery a month before her due date. And miraculously, her baby was born alive, a little girl weighing just four pounds, who spent several weeks in our neonatal unit and went home healthy. I would see Triphonie and her daughter from time to time around Kibuye, her daugh
ter usually wearing an amazingly frilly party dress, both with big smiles on their faces. Do I remember all of my patients and their stories? Honestly, no, but Triphonie’s face and her story are indelibly burned in my memory.
Now, fast forward five years. It was just another OR day for me that Thursday morning in March…I had a list of C-sections to do that had been scheduled by my generalist colleagues. And I walked into the OR, and there was Triphonie getting her spinal anesthesia and smiling at me. She had come for her 6th pregnancy, a repeat C-section, and I was able to deliver her second living, healthy baby girl (full term this time). I asked my intern, who was doing the C-section with me, to translate to Triphonie how excited I was to be here, how thankful I was that she had two babies now, and that I still remembered all of her story. My intern, Patricia, said to me, “I remember her too. I was the medical student who cared for her baby in the NICU.”
It’s hard to explain how profound and impactful this is for me, on so many levels. First of all, this is a lady whose losses were incredible, and yet here at Kibuye, she received hope and ultimately new life in the form of her two daughters. She persevered, she tried again, and God put us in the right place at the right time to be able to participate in that gift of resurrection and redemption. In those moments when we’re stuck on that fourth pregnancy, the loss and the death and the brokenness (not unlike Good Friday), I have a story to cling to now to remember that this is not the end. Not for Triphonie, not for me. Sometimes we get to see the curtain pulled back and witness the NEXT pregnancy, the success, the miracle. The Easter Sunday. Sometimes we don’t see it, but it’s always going to come in some form or another. And this story helps me remember that.
Secondly, we’ve been in Burundi for nine years now. We came in with so many dreams and ideas and plans. Things have been infinitely harder than anticipated, or things have been harder in unexpected ways. Things haven’t always looked how we thought they would. But still, nine years later, our team is still here. And that nine years of constant presence and partnership with our Burundian colleagues means that sometimes we can look back and see how changes have come, slowly by slowly. Sometimes I can be part of someone’s story in a way that I couldn’t have been in we had only stayed a year or two. For Triphonie, I’ve had the chance to treat her during three different pregnancies over 7 years. That continuity is amazing to me. Or in another aspect, there was no NICU when we arrived nine years ago…there were cardboard boxes at the foot of the mom’s bed for the preterm babies. Triphonie’s baby is alive because of care provided by our competent NICU staff and locally made equipment like incubators.
Finally, perhaps my favorite part of the story was Patricia’s involvement. Not only did I have continuity with Triphonie, but Patricia had gotten to know her five years earlier as a medical student, and now here she was doing a C-section as one of our stage professional interns. Our team has been able to teach and train now hundreds of students at multiple and progressive levels, impacting health care throughout the entire region. All the stories that have impacted me….have also impacted other Burundian doctors as well. They remember these stories of hope and resurrection and redemption, too.
So on we go, in this Easter world where there is a promise of already and challenge of not yet. I am so grateful for the chance to reflect back on these stories, which give me hope for the road ahead. The tomb is empty. Death has been defeated. We wait with expectation.
13.4.22
Hip hip hooray for medical education
(by Ted John)
A few months ago, I wrote a post on medical education and my
experience organizing a 2-week dental course for the medical students, which
you can read more about here. It was the first time teaching such a course at
our hospital and the first time for me to coordinate/organize a course. Since
we don’t have any dentists on site, teaching was done exclusively through audio/video
recordings and live video conferencing.
Fast forward a few months, and I have now finished coordinating
a new course on orthopedics and trauma. Here’s a table to give you an idea of
how they were similar and different, at a glance.
|
|
Dental |
Ortho/Trauma |
|
Number of students
enrolled |
46 |
52 |
|
Duration of
course |
2 weeks |
5 weeks |
|
Number of
instructors |
3 |
6 |
|
Number of (different)
lectures |
9 |
29 |
|
% of lectures
taught in English (PPT slides in French) |
78% |
26% |
|
Method of
instruction |
tele-education |
in-person (some
distance learning) |
Of course, there are a number of other differences. For
example, the scope of the ortho/trauma course was broader, but more related to
general surgery (at least as it pertains to trauma). Thus, while it would be ideal for
orthopedic surgeons to teach the more strictly ortho topics, we did the best
with what we had in terms of available expertise. In what other context could
you imagine an ortho/trauma course taught by a motley of 4 general surgeons, an
ER doctor, and a visiting orthopedic surgeon? 😄
 |
| Lecturing in our newly renovated classroom |
Another big difference was that not all students were
present for the in-person instruction at Kibuye. At any given point in time
during the course, there were 8-16 students doing clinical rotations off-site
in Bujumbura. As a result, it required more effort and coordination to ensure
that these students could have timely access to recorded lectures and
corresponding slides. The usual routine was that as soon as an instructor finished
giving their lecture, they would send me their recorded audio file, which I would
then upload to Dropbox (along with their slides). Then there’s the logistics of
administering quizzes and exams in two locations simultaneously, getting scanned
copies of the completed off-site quizzes, and grading and reporting all students’ results
in a timely manner. Doing this in the US with high-speed internet and ubiquitous
Wi-Fi would be challenging in and of itself, so accomplishing this in our
context is nothing short of incredible.
 |
| Medical students taking one of their weekly quizzes |
Here’s a condensed list of the content we covered:
• ATLS/Burns
• Trauma of the spine and chest
• Trauma/fractures of the upper extremities (shoulder, humerus, elbow, forearm/wrist, hand)
• Trauma/fractures of the lower extremities (hips, femur, knee, ankle)
• Musculoskeletal infections and tumors
• Differences in the pediatric population (plus congenital abnormalities)
 |
| Skeleton models of bones and joints were available for students throughout the course |
We’re also thankful for Joel Post, an orthopedic surgeon who visited for 2 weeks during the middle of the course. We intentionally planned the course to correspond with when he was around so that we and the students could benefit from his expertise. With Dr. Post’s fellowship training in orthopedic oncology as well as traumatology, he was the perfect person to give the lectures on osseous tumors and ankle fractures (which I view as generally more complex both in terms of injury patterns and management). As I sat in the back of the room listening to him, with stories of patients from his own current clinical practice, I couldn’t help but think, “Wow, this is so interesting. I wish Joel could teach all the ortho lectures!”
 |
| My family with Joel just before his return to the US |
Overall, though, I’m quite pleased with how the course
turned out, and I think the students learned a lot. As with the dental course,
I recognized the top performing students, but this time with little bags of calcium
supplements (tums) for fun. I even trialed an electronic post-course survey through
google forms to solicit feedback, the template for which others can continue
using in future courses going forward. In response to the question of what was
the best part of the course, a good number of students said “everything”. Yet, I
know there’s room for improvement, and will take to heart the students’
suggestions for the next time this course is taught again in a couple years. For
now, I can redirect my attention elsewhere, perhaps in helping with the start
of a surgery residency training program in the coming months. Tibia continued...
 |
| Group photo with the Kibuye cohort of students at the end of the course |
8.4.22
4 Brief Cases from a Surprisingly Encouraging Clinic
(from Eric)
(Note: These windows into my life and work are undeniably medical. My experience is that the non-medical folks divide pretty quickly into the camps of "Boring!" and "So fascinating!" I offer this in hopes that it will be helpful to medical readers as well and those non-medical folks who find such things interesting.)
For many years, Wednesdays have been my day for offering Internal Medicine specialty consults. It started as a small clinic, and has steadily gained steam to the point that it's quite a long, busy day every week. I have (somewhat) jokingly also called it my "bricks without straw" clinic, or alternatively my "everyone gets amitriptyline" clinic. Suffice to say that managing complex chronic medical diseases in our context is often really hard. Some days are quite exasperating, but there are usually some people that I feel that I've been able to really help. Aside from that, I always have a post-graduate intern doctor with me and a couple medical students, so there are also unique educational opportunities.
This past Wednesday was a public holiday in Burundi (commemorating the death of President Ntaryamira in 1994, who was shot down in a plane with then Rwandan President Habyarimana). Technically, this would mean I wasn't seeing consults like normal, but I figured I might as well be there. It turned out to be a pretty busy day, and most of the people who came had been given a follow-up appointment for that day after past visits or past hospitalizations (because we forgot it was a holiday). In the end, there were a number of really encouraging moments, and I thought I'd share 4 of them, both for the purposes of encouragement and interest.
1. Leonidas is a 35 year old man who was hospitalized on our service a couple weeks ago. He came in with whole-body swelling (imagine an enormously swollen person and then double that) along with trouble breathing that needed oxygen therapy. His swelling seemed to be from a severe kidney disease (mixed nephrotic/nephritic for medical folks), but his lungs were super wheezy, which
seemed weird (though not impossible) for the expected "water on the lungs" that seemed most likely for him. We were giving him huge doses of IV Lasix (to try to help him pee off the excess fluid) with absolutely no effect. We had a thought that he could have a rare inflammatory vasculitic syndrome that was causing his lungs and kidneys to both fail together. In absence of any tests to confirm that, and with his life obviously threatened, we started him on steroids. His lungs were getting better, and he got off oxygen, but given our failure to get his swelling down at all, we recommended he go to Buja to see a kidney specialist, and he agreed.
Fast forward to clinic, a man walks in, smiling at me, and I don't recognize him in the slightest. It's Leonidas, whose kidneys started working, and our medicines caused him to lose OVER 25% of his body weight in fluid. He's walking around and feels quite good. I'm shocked, and we laugh together at the surprising goodness of it all. Turns out he didn't have any money to go to Buja, so he's been haunting the hospital grounds for a couple weeks, waiting to see me in clinic. I was afraid all our medicines could have hurt his kidneys more with such a dramatic response, but they are almost back to normal. We adjusted his meds, and set him up to come back in a month.
2. Gloria is a 48 year old woman hospitalized last month with new onset diabetes who came in in a coma from diabetic ketoacidosis (DKA). Despite the low mortality rate of this problem in the US, most of these patients used to die here. Starting around 3-4 years ago, we found a way to reduce the cost of blood sugar testing at the bedside, which enabled us to test more frequently, and patients generally do much better. Gloria had the added blessing of showing up when Carlan was in the ER, which meant a quick diagnosis and initial treatment. She went home after about 5 days. We stopped her injectable insulin (super hard to maintain in a village home with no electricity), and hoped her metformin pills would do the trick. They're working beautifully.
3. Esperance is a similar lady, but she's only 16. She also came in with new diabetes and a coma with DKA. We hemmed and hawed about stopping her insulin to try pills. It shouldn't work. She should be dependent on injectable insulin. But here's the funny thing. Here in Burundi, I see numerous young skinny patients with diabetes who can be well treated with pills for years. Given how huge of a difference that makes in their lives in this context, we usually try and usually succeed. But 16 years old?
As it turns out, I wasn't around the day she came back, and our Burundian doctors tried the pills. Their gamble paid off, and she is doing great.
4. Charlotte is a 52 year old lady that I diagnosed with severe heart failure (ejection fraction of 15%) in 2017. She easily would have died around that time without intervention. She has been incredibly faithful in taking her medicines and coming back every 6 months to see me, even though she feels totally fine and is able to farm in her fields like everyone else. We rescanned her heart, and it's still obviously sick, but significantly better than 5 years ago. She'll continue a half-pill twice a day and we'll see her again in October. We thanked God together for the past 5 years of health that she has received.
 |
| A view of my consult room. I didn't see this lady last week, but she's been seeing me for years and always comes at the end of the day full of smiles and joking. She's my biggest fan. |
6.4.22
Kibuye Weather Station
by Michelle Wendler
We are happy to unveil the new Kibuye Weather station (thanks to a combined gift from our family to Carlan).
Link to the weather station:
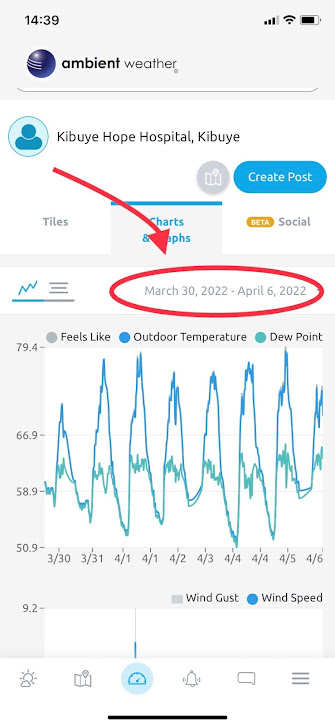
Here are a few pictures to help you navigate the info you can get. Here's what the most current weather would look like:
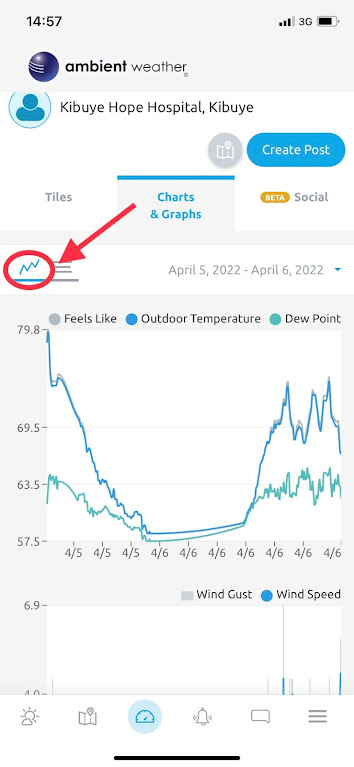
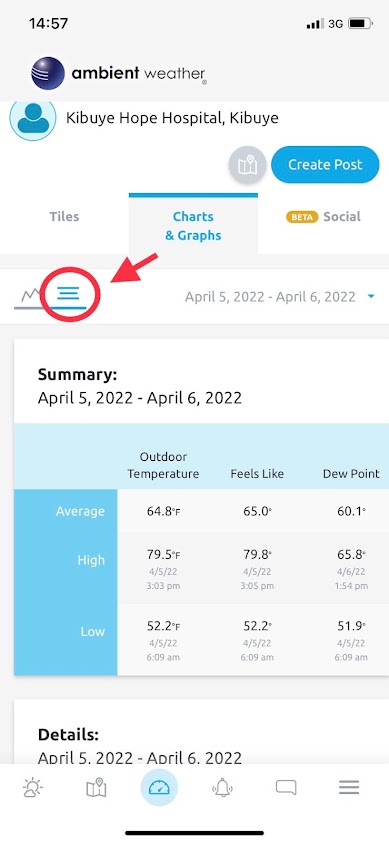
Under charts and graphs you can see what the last 24 hours has been, or change the date (see example below) to see data for the last week, month, or even longer. We installed the station the end of February, so we only have been collecting data since then.
If you like graphs:
If you like tiles:
Working hard during a thunderstorm:
And there are many more features, I just highlighted a few. And you can even download the Ambient Weather app (see picture below) to have the data easily accessible to your phone.
One final note, if you ever check and there's no recent data, that means we don't have power and the battery backup has run out of juice as well. But once power is restored, then the data should be available again.